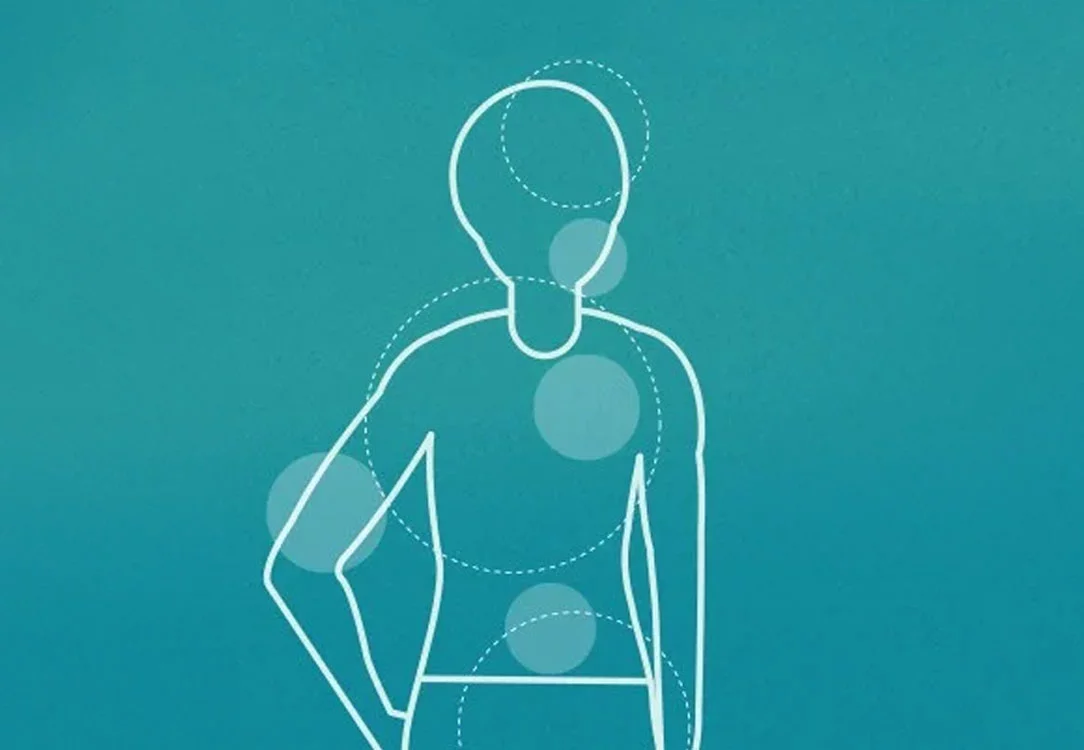
Your oral and overall health have a definite relationship, which we call the Mouth-Body Connection (MBC). With over two decades of research on the topic, we know much of this link has to do with inflammation and harmful bacteria in the mouth that affect other parts of your body and any systemic conditions you might have.
Inflammation and Your Overall Health
There are two types of inflammation, acute and chronic. Acute inflammation is a site-based response that results from an injury or threat from a toxin. Chronic inflammation occurs when the cells attack a part of the body without threat and create an inflammatory response that never goes away. Chronic inflammation can interfere with your body’s systems and keep them from doing what they should.
Inflammation and Your Oral Health
In addition to your other systems in the body, inflammation has detrimental effects on your oral health. Bacteria in the oral cavity that threaten the gums trigger an inflammatory response. This response can trigger the early stages of gum disease or periodontal disease. If the inflammation remains and is left untreated, it can worsen, leading to swollen gums, gum tissue loss, gum recession, infection in the supporting bone and jaw joint, and tooth loss.
To learn more about inflammation and its effects on your overall and oral health, read our blog Chronic Inflammation Blog
Inflammation and the Increased Risk of Diabetes Connection
For example, research suggests inflammation in the gums, a hallmark of gum disease, increases the risk of developing diabetes by nine percent. In addition, if you have many missing teeth, 15 or more, your risk of developing type 2 diabetes jumps to 21 percent. The American Diabetes Association indicated in 2017 that one in five people with severe gum disease had type 2 diabetes and didn’t know it. Salivary Diagnostics from a saliva test administered by your Smile Generation dental team can report the glucose levels in your mouth.
Read our other blog to learn about the link between diabetes and your gums.
Inflammation and the Increased Risk of Heart Disease Connection
The connection here is the five bacteria found in the mouth, which we sometimes describe as the “5 biggest, baddest bacteria.” (To learn the five names of the bacteria and other relationships involved in the MBC, please download our eBook, “32 Reasons to Learn About the Mouth-Body Connection.”) These bacteria are the periodontal pathogens that can travel from the mouth throughout the body, wreaking havoc on your systems as they go.
To learn more about this connection between gum disease and your heart read our blog.
Inflammation and the Increased Risk of Alzheimer’s’ and Dementia
There also exists a relationship between periodontal disease and Alzheimer’s. Like the other systemic conditions, gum inflammation increases the risk of developing brain diseases like Alzheimer’s and Dementia. This increased risk results from the bacterium entering the bloodstream and traveling throughout the body, including the brain.
Tooth loss is often a harbinger of future brain health decline. For example, losing more than half your teeth by age 60 makes you more than double your risk of Alzheimer’s. Also, tooth loss due to gum disease often happens 20 to 30 years before dementia. In addition to these brain health declines, poor oral health can affect cognitive function and mental health.
To learn more about the connection between your mouth and brain read our blog.
Inflammation in Gums Effect on Women’s Oral Health
Periodontal Disease and Women’s Health
In particular, hormone levels increase blood flow to the gums, which can lead to bleeding and swelling. In addition, decreases in hormone levels, which occur with menopause, cause dry mouth as saliva levels drop, creating an environment where bacteria can thrive and gum disease worsens. Some women also feel a burning or tingling sensation in their mouths during menopause.
For example, pregnancy is a time when these effects are pronounced. Many women develop gum disease due to the changing hormone levels throughout pregnancy. These bacteria in their mouths can then travel throughout the body. Research has linked this bacterial load to adverse pregnancy outcomes, like low birth weight. There is also a connection between mothers who have gum disease and pre-term labor.
To learn more about women’s oral health at all life stages read our blog.
Gum Health: The Link Between All of Them
To learn more about the connection between Periodontal Disease and the Mouth-Body Connection, read our blog
Find a Dentist Near You
For more information or to find a Smile Generation dentist near you use our Find a Dentist Tool.
Find your trusted, local dentist today!
Smile Generation blog articles are reviewed by a licensed dental professional before publishing. However, we present this information for educational purposes only with the intent to promote readers’ understanding of oral health and oral healthcare treatment options and technology. We do not intend for our blog content to substitute for professional dental care and clinical advice, diagnosis, or treatment planning provided by a licensed dental professional. Smile Generation always recommends seeking the advice of a dentist, physician, or other licensed healthcare professional for a dental or medical condition or treatment.